Talk:Atrial fibrillation/Archive 1
| This is an archive of past discussions. Do not edit the contents of this page. If you wish to start a new discussion or revive an old one, please do so on the current talk page. |
| Archive 1 |
What this article needs
This article needs:
- Some basic electrophysiology - where do action potentials originate, what perpetuates them, what determines whether the impulse is conducted by the AV node.
- A good list of risk factors
- Images of 12-lead ECGs with perhaps an example of PAF or atrial flutter
- Links to international guidelines for treatment, anticoagulation, cardioversion and surgery/EP ablation
- Burden of disease in the Western world, contribution to stroke incidence, perhaps also see if there are studies on the cost of anticoagulation services for AF and whether rhythm control could modify this!
- Is there historical information on the disease entity, eponyms etc.
I'll try to help along on this one! JFW | T@lk 15:34, 21 December 2005 (UTC)
- It's a good framework, for sure. There's a lot of jargon and not many references. I think that the causes section needs to be converted into text. Lone AF is absent and more could be said about structural heart disease causing AF. The role of AF in precipitating failure in MS/AS, etc. should also be mentioned. I've been on the cardiac step-down unit the last few weeks (the Smack-down) but should now have some time in the next few weeks to contribute. InvictaHOG 23:36, 26 December 2005 (UTC)
- Autonomic nervous system influences Bob K31416 (talk) 17:04, 14 June 2008 (UTC)
- Status of approval by EU and USA regarding the use of various drugs and devices for treating AF; off-label use --Bob K31416 (talk) 19:47, 15 July 2008 (UTC)
- I was advised by my doctor of a technique to end an A-Fib episode and it works - to take a deep breath and bear down like pilots do in the G-force machine to keep from passing out. This works, but I have seen no reference to this very helpful technique in any of the A-Fib literature on the net. Perhaps a medical professional could write something on this please? 70.72.26.188 (talk) 07:33, 13 September 2008 (UTC)
- See Valsalva maneuver. --Bob K31416 (talk) 11:30, 13 September 2008 (UTC)
- Works for some. Others, like myself can sometimes get out of afib by hard exercise or even coughing, if done quickly after onset(or just getting damn angry, lol). Sex works for others. —Preceding unsigned comment added by 58.178.191.215 (talk) 07:41, 14 January 2011 (UTC)
- See Valsalva maneuver. --Bob K31416 (talk) 11:30, 13 September 2008 (UTC)
section 6.5.1 anti-arrhythmic agents
says AF can be controlled with Na+ chan blockers (Class I) or K+ chan blockers (Class II). but class II = beta-blockers, and K+ block = Class III. So is the treatment with K+ block or class II? I would guess at K+ (Class III) but guesses arent encyclopaedic —Preceding unsigned comment added by 87.194.78.179 (talk) 17:48, 20 May 2009 (UTC)
"Maze" v. "maze" procedure
I left a similar comment on Jamesmcclelland's page. I've lowercased the "maze" in "Cox maze procedure" given that maze is not a proper noun. It would be akin to capitalizing "forceps" in "Debakey forceps" or "clamp" in "Kocher clamp." A casual pubmed search shows that maze is also in lowercase. Andrew73 02:31, 28 December 2005 (UTC)
jamesmcclelland here. It's been used both ways, but it seems that James Cox, who invented the procedure, prefers that "maze" be capitalized to "Maze". I agree that this doesn't make too much sense, but that's how it has usually been done. See his recent publication for instance:
Cox JL. The Role of Surgical Intervention in the Management of Atrial Fibrillation. Tex Heart Inst J. 2004; 31(3): 257–265. PMID 15562846
I left it uncapitalized anyway, rather than go around and around.
- Thanks for finding the reference. While Cox may have capitalized "maze" in the original article, the majority of the published literature from what I've seen uses it in the lower case version. It seems that the capitalization is a little bit idiosyncratic, almost an affectation! Andrew73 20:19, 2 January 2006 (UTC)
- Actually, I think it's an "attibution" thing; that is, "maze" is relatively generic, whereas "Maze" refers to the procedure he developed. My impression of how the terms are used is that if it's an actual Cox Maze (that is, if Cox was associated with it) - such as the original Cox Maze, the Cox Maze II, the Cox Maze III, or the (can you believe it) Cox Maze IV, it is capitalized. Also, *his* version of the MiniMaze. When others make variations on the theme, such as the various "minimaze" procedures, it is not capitalized. I think that's why you are seeing that much of the literature is uncapitalized.
- Here's my position: Cox is indeed the originator of this field of arrhythmia surgery for AF, and I think that it's reasonable to recognize that by things like capitalizing the original Maze(s) as he does. I'd leave other mazes lowercase. This is consistent with the literature in my opinion. What do you think? jamesmcclelland 22:48, 2 January 2006 (UTC)
- Interestingly, while "maze" is capitalized in the Texas Heart Journal reference, there are multiple other references authored by Cox where "maze" is left uncapitalized, e.g. PMID 8215657. I'd be curious to hear what others think! Andrew73 22:58, 2 January 2006 (UTC)
- Here's my position: Cox is indeed the originator of this field of arrhythmia surgery for AF, and I think that it's reasonable to recognize that by things like capitalizing the original Maze(s) as he does. I'd leave other mazes lowercase. This is consistent with the literature in my opinion. What do you think? jamesmcclelland 22:48, 2 January 2006 (UTC)
- We could flip a coin! InvictaHOG 02:31, 3 January 2006 (UTC)
- Hmmm... coin flip via internet? The reference you (Andrew73) have cited is from 1993, after his first 75 patients. It was substantially later that other "Maze-like" procedures began to be published and the issue of distinguishing between these procedures became important. jamesmcclelland 04:12, 3 January 2006 (UTC)
- Flip the coin here: http://www.random.org/flip.html Now we only have to choose which coin to flip... :) --WS 04:38, 3 January 2006 (UTC)
- I will wait a few days and see if anyone else weighs in. jamesmcclelland 07:25, 3 January 2006 (UTC)
- I'm having a terrible time convincing people that the procedure was not co-invented by Dr. Maze, and that MAZE is not an acronym for something. Leaving "maze" uncapitalized helps people understand that it's called a Cox maze procedure because it's like a maze.--Mark D Hardy 16:40, 19 May 2006 (UTC)
Lone afib
I added a little regarding LAF and made some stylistic changes. --DocJohnny 10:19, 30 December 2005 (UTC)
Symptoms
That AF can be asymptomatic is implied in the text, but I felt it would be better to directly state this as it may not be clear to a lay reader --Mattopaedia 07:42, 31 December 2005 (UTC)
Electrocardiogram
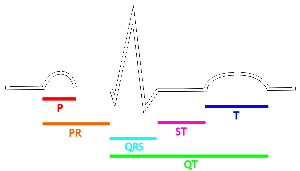
P=P wave, PR=PR segment, QRS=QRS complex, QT=QT interval, ST=ST segment, T=T wave.
Is it worthwhile including this image from electrocardiogram (or something like it) to give the reader some instant idea of what is meant by "absence of P waves" etc? --Mattopaedia 07:49, 31 December 2005 (UTC)
- I say, be bold and add it! Though it might be better if we duplicated it into several cardiac cycles to show its regularity InvictaHOG 22:55, 2 January 2006 (UTC)
More about classification and treatment
I have clarified classification based on ACC/AHA guidelines. But more needs to be done to organize the treatment section, especially in regards to initial episode vs. recurrent. I will try to tackle those later. --DocJohnny 17:54, 31 December 2005 (UTC)
Also, I have added references in the forms in in text links, I am unfamiliar with the format used for endnotes. Perhaps a kind bot will assist in formatting. --DocJohnny 13:40, 1 January 2006 (UTC)
External Links
Hi, I am new to this site but I have found a great website that offers the most in-depth, physician reviewed content on Atrial Fibrillation that I have seen. I tried to add the link but was told it would be removed---and it was. The link to the content is here: http://www.medifocushealth.com/CR004/atrial_fibrillation.php---If you (like me) think its good content, can you tell me how I can add this resource so others may benefit? Thanks.
- While the content is of reasonable quality, it is supported with Google ads. Most of the material on the AF page on Medifocushealth should actually already have been incorporated into this Wikipedia article. In that sense, I do not support inclusion of the link.
- I see you are alphabetically linking all the pages from that site on Wikipedia. This is spam and I would strongly discourage you from doing this. Wikipedia is not a way to improve site traffic. JFW | T@lk 05:10, 21 December 2006 (UTC)
In the illustration of pathophysiology I believe that the illustration is incorrect in that it shows the wave propagating down the heart. The impluse actually goes down the Bundle of His and then the depolarization of the heart begins the bottom of the heart and works it way up. The squeezing of the heart must begin from the bottom if you think about it as the exit valves are not at the bottom of the heart but roughly in the middle. I would appreciate further commentary from an expert electrophysiologist. Thomas
Normal vs AFib conduction image
This is in response to a stray post under External Links talk. Under Pathophysiology, the GIF comparing normal conduction v AFib conduction is misleading. This appears to be an artists rendition rather than a medically acurrate and informative image. The conduction goes from the Sinus node to the muscle of the atria to the HIS bundle as shown, but then goes down the Purkinje Fibers down the center of the Ventricular septum. It then activates through the heart muscle from the Apex up to the base of the ventricles. I'll try to find an Image or set of images that would be more accurate.Nbrysiewicz 22:52, 24 March 2007 (UTC)
Here is a GIF of normal sinus rhythm. I don't know how to edit GIFs otherwise I would have made an example of AFib using this GIF. I need help to make this page more accurate. If anyone can, please replace the images with corrected GIFs. http://en.wikipedia.org/wiki/Image:ECG_Principle_fast.gif Nbrysiewicz 00:59, 25 March 2007 (UTC)
Afib vs sinus
Just looking at the example of supposed Afib I don't know... Without calipers and a longer tracing, it looks more like some kind of block at first glance, the irregularity is too regular. Even if it is Afib it certainly is not a classic looking Afib. I'm going to see if I can find a better one unless someone else can first. - Dan D. Ric 01:30, 25 March 2007 (UTC)
- Holy cow. Looking again at the larger image. This is most definitely NOT a tracing of Afib! The r-r intervals, except for the missing beats, are EXACTLY regular. I hope whoever decided this is Afib is never my cardiologist. The image should be removed till a real example of Afib is found. I'd do/say more except it's time for me to go to work. -- Dan D. Ric 01:39, 25 March 2007 (UTC)
- The tracing appears to be atrial flutter with variable block. The rate is 150 with occasional dropped beats - the classic rate for atrial flutter is 150. I can convince myself of the sawtooth waveform as well. The morphology of a.fib / a.flutter is different, but the treatment is essentially the same. Dlodge 14:11, 25 March 2007 (UTC)
I'm glad to see someone else looking at this but I don't agree. Having only one lead to look at is a hindrance (as is me being out of practice since I haven't worked in cardiology for 3-4 years) but I'm not sure about a flutter, I don't see the sawtooth. How about some kind of accelerated junctional or junctional tach? Some of those QRS complexes look to have a retrograde P. Whatever it is, it is certainly not a good example of either Afib or flutter. - Dan D. Ric 15:14, 25 March 2007 (UTC)
- Certainly a somewhat regular ventricular response. Atrial rhythm is unclear. Either atrial fibrillation with regular noise (electrical or mechanical artifact) or an atypical flutter with noise. I agree that the regular ventricular response makes things confusing. Someone's certainly got a better image, right? Ksheka 13:22, 11 May 2007 (UTC)
How about this image instead of the one currently in the Electrocardiogram section? I think it is a more typical atrial fibrillation albeit a bit slow. This is a 103 year old female with CHF and history of a-fib with RVR, on Digoxin, Diltiazem, Metoprolol, Furosemide and Potassium. Note the variations in the R-R and the numerous P-waves.

Dan D. Ric (talk) 16:14, 27 March 2009 (UTC)

Here's the figure from the article. Comparing the nominal AF trace (upper) with the NSR trace (lower), one could also interpret the difference as extra beats in the upper trace, rather than missing beats. Also, there seems to be a diversity of AF and perhaps some patients may only appear to be close to NSR with regard to R-R, but not quite. It might be helpful if someone knew of an article that discusses the diversity of AF ECG's. --Bob K31416 (talk) 18:11, 27 March 2009 (UTC)
- Just looking at the spacing of the QRS's, the first thing I would think is "Wenckebach," but whatever is going on in the baseline is too noisy to really tell. I think I may be seeing some P-R interval lengthening but it's too hard to pick out the P-waves in all that jumble. Dan D. Ric (talk) 23:02, 27 March 2009 (UTC)
- First of all, don't p waves refer to the element of an ECG that corresponds to a coordinated contraction of the atria, not quivering, as appears to be happening in the AF ECG.
- Secondly, how can you see a lengthening of the P-R interval (Wenckebach) if there aren't any p waves, much less a P-R interval? --Bob K31416 (talk) 14:17, 28 March 2009 (UTC)
Well, generally there are P-waves in A-fib, they just aren't all conducted to the ventricles. In a 2:1 or 3:1 flutter, which is a type of A-fib, only every other or every third P-wave is conducted and the rest blocked. Secondly, I don't believe the tracing currently in the article is A-fib anyway. There are what I believe to be P-waves but it is too hard to pick them out of the surrounding noise to be certain.
Anyway, the point is, is the one I uploaded a better example then what we have now? I'd like to hear some more opinions. Dan D. Ric (talk) 16:10, 28 March 2009 (UTC)
- Here's an excerpt from an AHA web page titled Atrial Fibrillation (for Professionals), "As a result, there is no contraction of the atria as a whole. Since there is no uniform atrial depolarization, there is no P wave. " --Bob K31416 (talk) 17:43, 28 March 2009 (UTC)
Thyroxine
http://archinte.ama-assn.org/cgi/content/abstract/167/9/928?etoc - thyroxine levels are independently associated with presence of AF, even when asymptomatic and in normal TSH. JFW | T@lk 08:30, 15 May 2007 (UTC)
Over 75
doi:10.1016/S0140-6736(07)61233-1 - over 75 some are concerned re bleeding risk. This study seems to put that to rest - it compares aspirin to warfarin in a non-randomised fashion (can't randomise for weekly INR checks) and found a 50% relative and 2% absolute risk reduction. JFW | T@lk 09:35, 12 August 2007 (UTC)
Copyediting
I'm doing a bit of a copyedit to the article. In particular, I'd like to get rid of any headers in level 4 or over (as per the WP:MOS). I've moved some material to relevant sections (e.g. "screening" is now a dedicated section). I've started referencing much content to the ACC/AHA/ESC 2001 guideline. We also have the NICE guideline which definitely needs to be mentioned too. JFW | T@lk 19:17, 29 August 2007 (UTC)
- I have been unable to completely eliminate use of level 4 headers. Some more content can probably be referenced to the ACC/AHA/ESC guideline. I will see if I can find this out in due course. JFW | T@lk 22:09, 29 August 2007 (UTC)
Organization of treatment section
I think the treatment section of the atrial fibrillation might benefit from different organization. What about:
- 6.1 Rate control versus rhythm control
- 6.2 Rate control
- 6.2.1 Acute rate control
- 6.2.2 Chronic rate control
- 6.3 Rhythm control
- 6.3.1 Conversion to sinus rhythm
- 6.3.2 Maintenance of sinus rhythm
- 6.3.2.1 Medications
- 6.3.2.2 Radiofrequency ablation
- 6.3.2.3 Surgery
With this structure, it reveals that we do not discuss acute therapy and also that we are not distinguishing between conversion to and maintenance of sinus rhythm.Badgettrg 14:58, 6 September 2007 (UTC)
- I will agree to any organisation that avoids the need for deep headers. Acute therapy may warrant a separate section (is there any evidence?) but I feel we have quite a lot of information on rate vs rhythm. I thought those agents that converted to sinus also maintained sinus, or am I being ignorant? JFW | T@lk 19:12, 6 September 2007 (UTC)
- A little while ago I rearranged the structure of the article to be slightly more straightforward. Today you changed it back without discussion. Why is that? JFW | T@lk 20:46, 6 September 2007 (UTC)
- Which part?Badgettrg 20:55, 6 September 2007 (UTC)
- I'm mainly referring to the reintroduction of level 5 headers, which I will not support on grounds of readability. I have removed them now, and agree with other modifications you've made. Never mind.
- Are you aware of any cultural references and QOL studies in AF? I have identified American Journal of Medicine 2006;119(5):448.e1-448.e19. JFW | T@lk 12:00, 7 September 2007 (UTC)
- cultural references and QOL studies in AF -> do not know of any
- I still have some trouble with the treatment section. For example, the paragraph 'In refractory cases, where none of the above drugs are sufficient' being in the rate control section and not having a section titled 'Rate control versus rhythm control'. I think you are wanting to organized based on available treatment modalities, whereas I prefer to organize around the clinical settings likely to arise - even though it means discussing a treatment in more than one section.
- The pros/cons of level 5 headers is interesting; so the discussion does not get lost, I am continuing it below in its own section.Badgettrg 03:47, 9 September 2007 (UTC)
Level 5 headers
Personally, I do not mind the version with level 5 headers if there are concepts that really nest that deep. I could not find any WP recommendations against using level 5 headers - though I may have missed something - I checked Wikipedia:Manual of Style (headings). Regardless, in searching for WP policy on this, I found an interesting technical compromise - Help:Section: Limiting the TOC. My reasons for using headers as needed are:
- A number of times, I have found myself and other authors, putting too much detail about a subtopic in page, not realizing that a page already exists that is devoted to the topic (see cluster of topics on low back pain). This duplication of content then snowballs to where we have two large texts in parallel on the same topic. It is time-consuming and nearly impossible to harmonize and maintain the separate sections.
- When I have watched students and residents reading Internet pages, I am impressed how often the answer is in front of them but they do not see it - in part because there the blocks of text are too large, or the text they want is not represented in the TOC. Two studies that somewhat support the advantages of sections are Answering physicians' clinical questions: obstacles and potential solutions and Using structured medical information to improve students' problem-solving performance. Unfortunately, these articles do not address how much nesting can occur before text and TOCs become unusable.
Two avoid these two problems, I would use 5 sections if they are needed. However, determining 'need' is difficutl. If your not liking level 5 is the effect on the TOC, what about Help:Section: Limiting the TOC? So we would use {{TOClimit|limit=4}} or even {{TOClimit|limit=3}}. While a second alternative is to use bold text in front of paragraphs, this precludes using tags such as {{main|warfarin}} to visually alert in readers and authors that more detailed content is available.
What about the following which I think avoids level 5 headers. This could be done with {{TOClimit|limit=4}} or even {{TOClimit|limit=3}}:
- 6.1 Rate control versus rhythm control
- 6.2 Rate control
- 6.2.1 Acute rate control
- (allows space for discussion that we currently do not have about using beta and ca blockers intravenously)
- 6.2.2 Chronic rate control
- 6.2.1 Acute rate control
- 6.3 Rhythm control
- 6.3.1 Conversion to sinus rhythm
- 6.3.1.1 Medications
- 6.3.2.1 DC Cardioversion
- 6.3.2 Maintenance of sinus rhythm
- 6.3.2.1 Medications
- 6.3.2.2 Radiofrequency ablation
- 6.3.2.3 Surgery
- 6.3.1 Conversion to sinus rhythm
I think this is a difficult topic to organize, yet this page is very good. When I look at UpToDate's content, it is rather disorganized with 21 chapters that have a-fib in the title.Badgettrg 03:47, 9 September 2007 (UTC)
- I think I can agree with the outline. An alternative for {{TOClimit}} is using the semicolon method. Prefacing a header with a ";" (instead of surrounding it with "=" signs) generates a bolded heading that doesn't show up in the TOC. JFW | T@lk 20:52, 15 September 2007 (UTC)
- For your consideration (From my presentation on the topic a couple months ago):
- 1. Epidemiology
- 2. Etiology
- 3. Classification
- 4. Sequelae
- 5. Pathophysiology
- 6. Mechanism
- 7. Evaluation
- 7.1 Minimal evaluation
- 7.2 Extended evaluation
- 8. Management
- 8.1 Anticoagulation
- 8.2 Rate vs. Rhythm control
- 8.2.1 Rate control
- 8.2.2 Cardioversion
- 8.2.3 Maintenance of sinus rhythm
- Ksheka 14:00, 17 September 2007 (UTC)
- For your consideration (From my presentation on the topic a couple months ago):
- Okay. I decided to be bold and changed the organization of the entire article based on my outline above. We'll still need 4-level-deep headers, but the organization works better in general. (Though I wasn't sure where to put History. :-)) FYI, I think there is still a lot to be written in many of the sections. Ksheka 02:20, 18 September 2007 (UTC)
Sequelae/Natural History
For what it's worth, I think we're missing out without a sequelae (or natural history) section of the article. Stroke is one thing to be mentioned. Tachycardia-induced cardiomyopathy is another. And of course death. It's all in the article (somewhat spread out), but casual readers may look for a section like that. Ksheka 12:06, 19 September 2007 (UTC)
Clinical medicine/Template for medical conditions
- Going by Template for medical conditions, ok to move Classification to the first section?
- Sounds like Classification should go before Diagnosis. Not sure if it should go before Signs and symptoms. First section is certainly reasonable for me. Ksheka 00:42, 20 September 2007 (UTC)
- Very good point about missing natural history. I think I would label this 'complications' and go after prognosis is the standard order. To me this is so important, we should lobby to get it added to Template for medical conditions so other topics benefit from this structure.
- Ok if I insert a section 6.6.6 for "Determining risk of stroke"?
Badgettrg 12:59, 19 September 2007 (UTC)
- I was thinking of a new 6.0 - Natural history, with stroke being 6.1 and risk of stroke 6.1.1. Ksheka 13:40, 19 September 2007 (UTC)
- This brings up a recurring conundrum for me: when a treatment decision is tightly bound to a prognostic calculation, where do you put the prediction rule for the calculation? In the prognosis section, or the treatment section, or the complications section, or the natural hx section? This one stumps me.Badgettrg
- Prognosis and natural history generally mean the same thing. I would put risk calculations in with them. That also means putting natural history/prognosis earlier in the article than treatment. (between Pathophysiology and Treatment in the current article) Ksheka 00:39, 20 September 2007 (UTC)
- This brings up a recurring conundrum for me: when a treatment decision is tightly bound to a prognostic calculation, where do you put the prediction rule for the calculation? In the prognosis section, or the treatment section, or the complications section, or the natural hx section? This one stumps me.Badgettrg
- Also, are we so bound by Template for medical conditions, or it just a gentle suggestion? I haven't been too active lately in wikipedia and wasn't sure if this was something that all medical articles were being refactored into. Ksheka 16:24, 19 September 2007 (UTC)
- Doubt we are bound, but I do not know. In some ways (having classification early) it helps much, but in others (prognosis/complications) it is not helpful to me in its current form.Badgettrg
- There is some flexibility on order. FYI, Wikipedia:Manual of Style (medicine-related articles) has superseded Template for medical conditions, and provides some guidance on these issues, under the header "Diseases/disorders/syndromes". --Arcadian 01:53, 20 September 2007 (UTC)
- Doubt we are bound, but I do not know. In some ways (having classification early) it helps much, but in others (prognosis/complications) it is not helpful to me in its current form.Badgettrg
Some sources
Prevalence of Diagnosed Atrial Fibrillation in Adults may be a better source for the "2.3 million" statistic. The mortality figure is well supported with PMID 11978585. I will add these sources in due course (i.e. when I've scoured the fulltext). JFW | T@lk 16:47, 24 September 2007 (UTC)
- I found this useful. JFW | T@lk 16:49, 24 September 2007 (UTC)
- I noticed a lot of references pointing to the guidelines. As you noticed, at least one of the references in the guidelines (to statistics) doesn't make sense. Probably better to cite the actual papers rather than the guidelines, right? Ksheka 19:50, 24 September 2007 (UTC)
- I refer to guidelines when there is a cornucopia of papers but little agreement, and where there are various approaches for treatment and priorities are needed. If the guidelines are based on systematic reviews, they are very useful indeed. Now that we have found a rotten apple, a newer reference is obviously needed. JFW | T@lk 21:31, 16 October 2007 (UTC)
LIFE EXPECTANCY
Could someone add a section to this article about life expectancies for sufferers? Thanks! —Preceding unsigned comment added by 124.171.95.93 (talk) 07:19, 30 September 2007 (UTC)
- I'm not quite sure if that data is available. It is going to be a number with a very wide margin of confidence, rendering it practically meaningless. Some people live with AF for decades, and others have recurrent debilitating strokes. JFW | T@lk 21:31, 16 October 2007 (UTC)
Assessment
I don't usually rate things above "B" for the WPMED project, but it seems to me that this might easily meet the Good Article criteria. Perhaps someone should look up the criteria and see whether it seems likely to survive a nomination. WhatamIdoing (talk) 23:32, 19 January 2008 (UTC)
Catheter ablation better
http://archinte.ama-assn.org/cgi/content/abstract/168/6/581 catheter ablation (CPVA) is better than rhythm control. JFW | T@lk 02:59, 25 March 2008 (UTC)
"Main article: " form needed?
After a number of section headings there is a reference to Main article. For example,
Electrocardiogram
Main article: Electrocardiogram
Atrial fibrillation is diagnosed on an electrocardiogram (ECG), an investigation ...
In the above excerpt, "Main article: Electrocardiogram" doesn't seem to be needed since there is a link to the electrocardiogram wiki in that section. Perhaps it should be deleted along with similar instances of "Main article: xxxxxx" in other sections where the link is provided to their respective xxxxxx wikis. I checked that all sections have appropriate links in their respective text. ( I added a link in the one case where there wasn't one in the section's text.) Bob K31416 (talk) 03:24, 19 May 2008 (UTC)
- The {{Main}} template should really only be used if it is a subarticle of the present one. JFW | T@lk 05:34, 20 May 2008 (UTC)
- JFW, Thanks for the info. After reading your comment and looking at {{Main}} and Wikipedia:Summary style it does appear that the {{Main}} template was inappropriately used since e.g. the article Electrocardiogram did not grow out of the present article Atrial fibrillation. For those interested, this excerpt from Wikipedia:Summary style gives more useful details of the proper use of the {{Main}} template,
- "Wikipedia articles tend to grow in a way which lends itself to the natural creation of new articles. The text of any article consists of a sequence of related but distinct subtopics. When there is enough text in a given subtopic to merit its own article, that text can be summarized from the present article and a link provided to the more detailed article."
- So I'll delete instances of the form "Main article: xxxxxx" that refer to wikis that were started before the present article and thus weren't originally in the present article. I'll look to see if the other "Main article" references were originally in the present article.
- JFW, Thanks for the info. After reading your comment and looking at {{Main}} and Wikipedia:Summary style it does appear that the {{Main}} template was inappropriately used since e.g. the article Electrocardiogram did not grow out of the present article Atrial fibrillation. For those interested, this excerpt from Wikipedia:Summary style gives more useful details of the proper use of the {{Main}} template,
- However, even if they originated in the present article, it still doesn't seem useful to use the {{Main}} template if there is a link to the spinoff article in the section's text. I'd appreciate any more of your thoughts. Bob K31416 (talk) 15:10, 20 May 2008 (UTC)
- I investigated whether any of the "Main article" references were originally in the present article. I found that almost all of the "Main article: xxxxxx" entries were made on 24Sep2007 by Ksheka. Also, I looked at the first instance of the referenced articles in their respective histories and the corresponding state of the AF article at that time for many of the referenced articles. Most likely all of the referenced articles did not first appear in the present article on AF so, with my previous remarks in mind, there doesn't seem to be any reason for keeping the "Main article: xxxxxx" entries. Bob K31416 (talk) 22:15, 20 May 2008 (UTC)
Classification
It appears to be difficult to achieve a well organized classification system for AF. This may be due to: the diversity of episode timing and termination characteristics; the diversity of category names and their definitions that have appeared in the literature; and the seemingly inevitable overlap of categories. Even the AHA/ACC/ESC 2006 Guidelines appears to have trouble with coherence in this regard. The part of those Guidelines that seems to have the simplest and most systematic attempt at classification is Fig. 3. From that figure comes the following classification system:
- First detected
- Paroxysmal - self-terminating, lasting less than 7 days
- Persistent - not self-terminating, lasting more than 7 days and terminated by intervention
- Permanent - not self-terminating, lasting continuously long-term (e.g. for a year or more) and termination by intervention either failed or not attempted
Additional categories come from the rest of the Guidelines' classification section:
- LAF
- nonvalvular
Currently, the AF wiki's interpretation of the Guidelines' classification system lumps together most of the major categories (paroxysmal, persistent, and permanent) into the one category "Recurrent atrial fibrillation". Furthermore, "Recurrent..." is too large a category compared to the "First detected..." category. So it seems reasonable to use the system in the Guidelines' Fig. 3 to replace the "Recurrent..." category in the AF wiki with the categories Paroxysmal, Persistent, and Permanent.
Also, in addition to the LAF category in the AF wiki, the category "Nonvalvular AF" should be mentioned in the Classification section since it is referred to later in the AF wiki, it is in the classification section of the Guidelines, and it appears in many other journal articles.
Finally, the use of the term "chronic" can be a source of confusion. It has been used to differentiate long-term episodes from short-term episodes but this can be confusing. The reason for the confusion is that one might reasonably think that the term "chronic" would apply to having short-term episodes frequently, over and over again, without an end to the paroxysmal AF.
Bob K31416 (talk) 01:49, 26 May 2008 (UTC)
Anticoagulation and Lone Atrial Fibrillation (LAF)
The first line of the section on Anticoagulation is:
“Patients with atrial fibrillation, even lone atrial fibrillation without other evidence of heart disease, are at increased risk of stroke during long term follow up.[1]”
One has to be careful interpreting the cited reference regarding LAF. It’s not clear that any of the patients who had strokes in the study were in the LAF category just before they had their stroke. In fact, they probably weren’t in the LAF category just before their stroke since on page 3453 of the article was the following statement,
“With total cardiovascular disease developing in more than 40% of the lone AF subjects at risk in this study, one would expect that underlying heart disease was present at the time of AF diagnosis, although clinically not observed nor unexpected in this group of older individuals.”
In other words, 40% of the subjects in the study who were supposedly in the LAF category at the beginning of the study either had or developed cardiovascular disease that moved them out of the LAF category. Furthermore, most if not all of the subjects who had a stroke were probably no longer in the LAF category just before the stroke but were among the 40% who had cardiovascular disease. Support for this assertion is a more current study of LAF which stated,
“Risk for stroke or transient ischemic attack was similar to the expected population risk during the initial 25 years of follow-up but increased thereafter (P=0.004), although CIs were wide. All patients who had a cerebrovascular event had developed > or = 1 risk factor for thromboembolism.”[2]
Thus, I feel that the phrase "even lone atrial fibrillation without other evidence of heart disease" should be deleted along with its associated reference, and the rest of the sentence should be modified to exclude LAF from the general assertion.
- ^ Brand FN, Abbott RD, Kannel WB, Wolf PA (1985). "Characteristics and prognosis of lone atrial fibrillation. 30-year follow-up in the Framingham Study". JAMA. 254 (24): 3449–53. doi:10.1001/jama.254.24.3449. PMID 4068186.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Jahangir A, Lee V, Friedman PA, Trusty JM, Hodge DO, Kopecky SL, Packer DL, Hammill SC, Shen WK, Gersh BJ (2007). "Long-term progression and outcomes with aging in patients with lone atrial fibrillation: a 30-year follow-up study". Circulation. 115 (24): 3050–6. doi:10.1161/CIRCULATIONAHA.106.644484. PMID 17548732.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
Bob K31416 (talk) 04:19, 4 June 2008 (UTC)
Autonomic Nervous System and AF
ACC/AHA/ESC 2006 Guidelines for the Management of Patients With Atrial Fibrillation Sections 6.1.6, 8.3.1.1, 8.3.2, 9.1.2
Autonomic nerve activity and atrial fibrillation
--Bob K31416 (talk) 18:05, 8 July 2008 (UTC)
Recent deletions of advertising
FHCPinehurst, Recent deletions of your contributions were due to advertising. The contributions were in a style that promoted a procedure, a doctor and a hospital. Please note the style of the rest of this wiki and try to conform. For example, doctors and hospitals aren't mentioned unless they are recognized pioneers, such as Cox and possibly Saltman, and it is the goal to describe procedures objectively in a way that doesn't try to influence readers to use them. Material in this wiki is not trying to sell readers on any product or service and it is the goal to present the material with a neutral point of view (WP:NPOV). Thank you. --Bob K31416 (talk) 19:06, 5 February 2009 (UTC)
However, I do agree that the basic info about the procedure should be in the wiki, without the advertising style, so I modified your contribution and added it. --Bob K31416 (talk) 20:07, 5 February 2009 (UTC)
I can understand not wanting any advertising, but why do you allow the link to Robert Wood Johnson University Hospital via "Minimally Invasive Surgical (Endoscopic) Procedures"? How is that an exception?--FHCPinehurst (talk) 20:48, 5 February 2009 (UTC)
- Thank you. I noticed that link too during my editing today and it is something to consider for possible deletion. I suspect that others have considered its informative value and decided to keep it, but I'm not sure of this. Please note that you are not being singled out and advertising has been routinely deleted in the past. Also note that I have since included the Ex-maze in the wiki without the advertising style. --Bob K31416 (talk) 21:46, 5 February 2009 (UTC)
- The link provides some nice pictures, which may aid people's understanding. Nonetheless, it does smack of aducation rather than education. Another thought - just to provide a more global perspective - is this procedure performed anywhere outside the US? Mattopaedia (talk) 12:29, 8 February 2009 (UTC)
- Re RWJ hospital link with useful diagrams- For the moment, I reduced the in-text link to a less prominent inline citation. Perhaps it can be replaced by a journal article that has similar diagrams for the minimaze. --Bob K31416 (talk) 13:41, 8 February 2009 (UTC)
- I just added to a citation a link to the fulltext version of a reference that contains diagrams, although the RWJ diagrams have some additional info. So the RWJ has become more deletable. Something to think about. And perhaps the RWJ diagrams are in another journal article. --Bob K31416 (talk) 22:22, 8 February 2009 (UTC)
Risk assessment
Would this modification of the recently deleted section Prevention and Risk Assessment, be acceptable?
- ==Risk Assessment==
- Even though one in four will develop atrial fibrillation in their lifetime, systematic studies of risk factors and prevention methods have been lacking. Patient features most closely related to future AF included age, sex, body-mass index, systolic blood pressure, treatment for hypertension, electrocardiographic PR interval, clinically important cardiac murmur, and heart failure. Devised from those risk factors, the scoring system assigned, for example, more points with advancing age (according to different scales for men and women) and more points the younger patients are at diagnosis of heart failure or a clinically important murmur.[1]
--Bob K31416 (talk) 01:29, 1 March 2009 (UTC)
P.S. I wasn't the one who put in the Prevention and Risk Assessment section under an IP address. --Bob K31416 (talk) 01:38, 1 March 2009 (UTC)
Prevention and risk assessment -- not to remove
Though it cited authority, the following section was once removed by an esteemed and prolific medical editor.
An informative removal note seemed to overlook risk assessment, though it was the major subject of the section and has lately taken a major step forward, as stated and substantiated in the removed text.
Second, the removal note expressed an opinion that there are no measures available for reducing risk if AF. This opinion (unsourced, though coming from a doctor) turns a blind eye to sourced "... tantalizing observational evidence that patients on statins or ACE inhibitors or those with high intake of omega-3 fatty acids may be at reduced risk of developing AF."
This observational evidence is the best there is, whereas the opinion that no measures exist for risk reduction does not appear to have any support at all.
Making available the best evidence currently available, albeit imperfect, may serve public health and does very little harm.
—Preceding unsigned comment added by 69.3.11.111 (talk) 18:20, 1 March 2009 (UTC)
- See above section on Talk page, Risk assessment, for a compromise. --Bob K31416 (talk) 18:27, 1 March 2009 (UTC)
Prevention and Risk Assessment
Even though one in four will develop atrial fibrillation in their lifetime, systematic studies of risk factors and prevention methods have been lacking.[2] Researchers for the Framingham Heart Study announced the first risk prevention tool in February, 2009.
- In multivariate analyses, baseline patient features significantly and most closely related to future AF included age, sex, body-mass index, systolic blood pressure, treatment for hypertension, electrocardiographic PR interval, clinically important cardiac murmur, and heart failure. Devised from those risk factors, the scoring system assigned, for example, more points with advancing age (according to different scales for men and women) and more points the younger patients are at diagnosis of heart failure or a clinically important murmur.[3]
Risk prevention is of value despite the lack of extensive study of possible prevention methods, in light of the
- ... tantalizing observational evidence that patients on statins or ACE inhibitors or those with high intake of omega-3 fatty acids may be at reduced risk of developing AF. ... [4]
—Preceding unsigned comment added by 69.3.11.111 (talk) 18:20, 1 March 2009 (UTC)
My take on "prevention"
The new Framingham score is interesting, and perhaps we should discuss it as part of the "epidemiology" section. However, it would be silly to suggest that anyone is actively "preventing" AF specifically by treating the risk factors. Rather, hypertension is treated to prevent stroke and ischaemic heart disease, etc etc. As such, there are no preventative strategies for AF. JFW | T@lk 20:25, 1 March 2009 (UTC)
- Your take is supported by the source too. Here's the rest of the context for the quote re "tantalizing", which I highlighted in bold, as I did points that are more negative.
- Benjamin acknowledges that the AF-risk scores are currently likely to be more useful in a research setting than in clinical practice; there aren't any accepted treatments for preventing AF that have randomized, controlled trial support.
- "We know a tremendous amount about how to prevent coronary heart disease. But the lifetime risk of atrial fib is about one in four, similar to the lifetime risk of heart failure, and we really know very little about how to prevent the onset of atrial fibrillation," she said.
- On the other hand, there is tantalizing observational evidence that patients on statins or ACE inhibitors or those with high intake of omega-3 fatty acids may be at reduced risk of developing AF. It might be reasonable, then, to explore those possible treatments in primary-prevention trials, which traditionally are conducted first in high-risk populations, Benjamin notes.
- Here's what the editor wrote.
- Risk prevention is of value despite the lack of extensive study of possible prevention methods, in light of the
- ... tantalizing observational evidence that patients on statins or ACE inhibitors or those with high intake of omega-3 fatty acids may be at reduced risk of developing AF. ... [5]
- It looks like the editor misinterpreted the source when the editor made the statement, "Risk prevention is of value... ". But like you suggested, there may be something useful to add to the Epidemiology section that doesn't involve prevention. I don't think the "compromise" suggestion that I hurriedly made above for a separate section, is suitable for the Epidemiology section in its present form. But there may be something on risk assessment that might be added to the Epidemiology section that would improve the article. --Bob K31416 (talk) 03:33, 2 March 2009 (UTC)
Speaking from the standpoint of a patient with long-standing paroxysmal AF, I can say that my current drug, propafenone (Rythmol SR)325mg has done the best job of preventing PACs; and when I did have an episode of AF, I converted to sinus rythm spontaneously (13 hours) and did not require cardioversion, as I had when I was taking acebutelol. My cardiologist had me on sotalol for a brief period, but the side effects and safety profile were unsuitable. Switching from beta blocker to propafenone has increased my resting heart rate from the high 70's to the high 80's, but my aerobic exercise capacity has improved with no increase in blood pressure. —Preceding unsigned comment added by Brucekdixon (talk • contribs) 16:02, 18 August 2009 (UTC)
The trouble with digoxin
Temporarily removed:
- Recent research questions the use of digoxin for AF. Increased mortality and faster transition from paroxymal to permanent AF by increased intracellular Ca ion overload can be the result of digoxin.[1] [2][3][4][5]
The sources are interesting, but I still suspect this amounts to WP:SYNTH. No official guideline discourages the use of digoxin for the reasons that it might induce permanent AF or increase mortality. The papers suggesting a risk of permanent AF are observational studies with indirect outcomes, and really do not prove much at all. The paper suggesting increased mortality looked at exactly 22 patients - not quite enough at all to draw any solid conclusions.
The British guidelines already discourage first-line use of digoxin apart from in the sedentary elderly. In the emergency setting, it is often the only suitable anti-arrhythmic if the patient is already borderline hypotensive and beta-blockers and calcium channel blockers would be unsuitable. JFW | T@lk 08:12, 17 April 2009 (UTC)
- Why not mention those guilines and the reason as many physicians routinely prescribe digoxin as a first line drug for otherwise healthy even young individuals? —Preceding unsigned comment added by 85.227.199.27 (talk) 13:30, 17 April 2009 (UTC)
- The paper from Uppsala [6] says:
- Conclusion The results suggest that long-term therapy with digoxin is an independent risk factor for death in patients with AF without CHF.
- The group of patients with AF and no CHF had a much larger cohort, 60,764, and you cannot just ignore their result. Digoxin cannot be put in the same group as beta- and calcium-blockers without any reservations. —Preceding unsigned comment added by 85.227.199.27 (talk) 18:45, 20 April 2009 (UTC)
- From the comments by JFW and 85.227.199.27, perhaps there should be something added to the article re JFW's remark, "The British guidelines already discourage first-line use of digoxin apart from in the sedentary elderly." --Bob K31416 (talk) 02:01, 25 April 2009 (UTC)
- Here's a link to the British guidelines. --Bob K31416 (talk) 13:40, 25 April 2009 (UTC)
What about: Digoxin should be restricted to patients with permanent AF and CHF when a beta-blocker or calcium channel-blocker cannot be used. —Preceding unsigned comment added by 85.227.141.186 (talk) 08:16, 3 May 2009 (UTC)
- From what I saw in the British Guidelines (i.e. NICE), CHF wasn't mentioned with regard to Digoxin. Use of Digoxin alone for permanent AF was limited to sedentary people when BBs and CCBs were contraindicated. However, when BBs or CCBs alone were indicated but inadequate, Digoxin in combination with a BB or a CCB was recommended. See p. 61. --Bob K31416 (talk) 21:39, 3 May 2009 (UTC)
So what is your suggestion? Would this solve your objections: Digoxin should be restricted to patients with permanent AF when a beta-blocker or calcium channel-blocker cannot be used. —Preceding unsigned comment added by GunnarK (talk • contribs) 04:15, 4 May 2009 (UTC)
- I would suggest: "- has limited use" so that the line in the article would be,
- Cardiac glycosides (i.e. digoxin) - has limited use
- I would also add the British guidelines citation to the AHA/ACC/ESC guidelines citation at the beginning of the Rate control section.
- "Atrial fibrillation: national clinical guideline for management in primary and secondary care" (PDF), National Collaborating Centre for Chronic Conditions, London: Royal College of Physicians, 2006, retrieved 2009-05-05
{{citation}}:|format=requires|url=(help); Cite has empty unknown parameters:|coeditors=and|coauthors=(help)
- "Atrial fibrillation: national clinical guideline for management in primary and secondary care" (PDF), National Collaborating Centre for Chronic Conditions, London: Royal College of Physicians, 2006, retrieved 2009-05-05
- P.S. Your last suggestion is not quite correct since digoxin can be used in combination with BBs and CCBs too. Also, you didn't mention the sedentary requirement. And in the AHA/ACC/ESC Guidelines, digoxin is used in other situations too. (BTW, they did mention HF there.) I decided to bypass these details since mentioning them would give undue weight to digoxin compared to BBs and CCBs.
- --Bob K31416 (talk) 14:57, 5 May 2009 (UTC)
- I just put the above suggestion in the article. --Bob K31416 (talk) 00:14, 9 May 2009 (UTC)
Thank you! I have been busy with other things. —Preceding unsigned comment added by GunnarK (talk • contribs) 08:57, 13 May 2009 (UTC)
OMIM
OMIM lists eight loci for familial AF (here). Do we need to link to all of them? JFW | T@lk 08:18, 22 August 2010 (UTC)
- Would this link be what you want? (Unfortunately it has #9 which I wasn't able to remove.) --Bob K31416 (talk) 18:36, 22 August 2010 (UTC)
Sodium Channel Blockers
A relatively new class of anti-arrhytmic medications called sodium channel blockers are used to treat atrial fibrillation. These seem to be somewhat toxic and are probably used when calcium channel blockers and beta blockers are ineffective. I think the best known sodium channel blocker for A-Fib is Propafenone, brand name Rhythmol. There is a Wikipedia article on Propafenone. I don't believe the article currently mentions this method of treatment. It's probably worthy of mention. 68.127.237.37 (talk) 21:57, 6 November 2010 (UTC)
New afib management
Circulation [7] Doc James (talk · contribs · email) 13:34, 21 December 2010 (UTC)
Unclear sentence
"The level of increased risk of stroke depends on the number of additional risk factors." What risk factors? Are they for a certain kind of strokes? Imagine Reason (talk) 06:11, 11 October 2011 (UTC)
Another unclear sentence
"A minimal evaluation should be performed in all individuals with AF." Sentence has two meanings. Will edit to reflect specifically what is intended. FeatherPluma (talk) 01:25, 6 November 2011 (UTC)
INR
I did not see a reference to the "INR" in this article, but I believe that this is assessed in sufferers of atrial fibrilation. As I am no expert on this subject (I shall confess that I do not even know what "INR" stands for!) I do not wish to edit the article. ACEOREVIVED (talk) 00:27, 14 March 2012 (UTC)
- It is only used if someone with atrial fibrillation is being treated with warfarin or another vitamin K antagonist. INR is used to determine the correct dose. JFW | T@lk 22:17, 6 March 2013 (UTC)
Cognitive impairment
Meta-analysis: here. JFW | T@lk 22:17, 6 March 2013 (UTC)
- This also: doi:10.1093/qjmed/hct129 (from QJM). JFW | T@lk 16:42, 8 September 2013 (UTC)
Lower target INR in the elderly
DocElisa (talk · contribs) suggested that we mention lower target INR in the elderly in view of a "redoubtable" risk of bleeding. This is supported with a primary research study, and also with the 2010 ESC guideline. The latter however says:
| “ | Whilst a lower target INR range (1.8–2.5) has been proposed for the elderly, this is not based on any large trial evidence base. Cohort studies suggest a 2-fold increase in stroke risk at INR 1.5–2.0 and, therefore, an INR <2.0 is not recommended. | ” |
The claim is therefore not supported by the most important reference. JFW | T@lk 21:42, 6 April 2013 (UTC)
- When I talk about geriatric patients I mean patients with ages >75 years old not >65. These patients have many risk factors like hypertension, they fall much more than young persons, they take most of the time anti-inflamatory drugs. In geriatrics an INR between 1.8 and 2.5 is enough to protect them. Most of these patients have chronic AF. The problem will be different if we face an intermittent AF. I think that this section can be expanded to explain better the problem. I´m always afraid when I see general clinicians treating 85 years old patients with warfarine with INR around 3 just because they have a chronic AF. Doc Elisa ✉ 11:13, 11 April 2013 (UTC)
- I don't disagree in principle, but the source contradicts what you were trying to say. JFW | T@lk 21:35, 14 April 2013 (UTC)
tPA antigen
tPA antigen levels predict cardiac/embolic events and death: doi:10.1111/jth.12213. Not for inclusion, but may become useful in stratifying risk. JFW | T@lk 12:46, 9 April 2013 (UTC)
WP:MEDRS
The use of WP:MEDRS to revert recent edits, while done in good faith, seems incorrect. First, this page has plenty of existing references to primary research; second, the secondary sources use to replace the original studies I cited do not cover the same content about the accuracy of the physical exam.
WP:MEDRS says primary sources ok if secondary sources do not cover the content. However, I only see WP:MEDRS used to remove primary sources.
How is arbitration arranged over disputed edits? Thanks. - Robert Badgett 05:14, 18 November 2013 (UTC)
- We use secondary sources to determine how much weight to give something. Typically in a main article we expect secondary sources. If you can get consensus than you can use it. Doc James (talk · contribs · email) (if I write on your page reply on mine) 05:28, 18 November 2013 (UTC)
I ask your advice about Medical algorithm for treatment of atrial fibrillation

I have placed this medical algorithm for treatment of atrial fibrillation in the Russian Wikipedia (Atrial fibrillation ru:Фибрилляция предсердий) — see the illustration on the right.
I want to ask. Maybe, this illustration should be placed into Atrial fibrillation also. Or will it be wrong? How do you think?
--Владимир Паронджанов (talk) 10:49, 11 April 2014 (UTC)
- ^ Steve Stiles Risk-Prediction Model for Future Atrial Fib Deepens Hopes for Primary Prevention from Heartwire — a professional news service of WebMD February 27, 2009 (Framingham, Massachusetts) http://www.medscape.com/viewarticle/588887
- ^ Steve Stiles Risk-Prediction Model for Future Atrial Fib Deepens Hopes for Primary Prevention from Heartwire — a professional news service of WebMD February 27, 2009 (Framingham, Massachusetts) http://www.medscape.com/viewarticle/588887
- ^ Steve Stiles Risk-Prediction Model for Future Atrial Fib Deepens Hopes for Primary Prevention from Heartwire — a professional news service of WebMD February 27, 2009 (Framingham, Massachusetts) http://www.medscape.com/viewarticle/588887
- ^ Steve Stiles Risk-Prediction Model for Future Atrial Fib Deepens Hopes for Primary Prevention from Heartwire — a professional news service of WebMD February 27, 2009 (Framingham, Massachusetts) http://www.medscape.com/viewarticle/588887
- ^ Steve Stiles Risk-Prediction Model for Future Atrial Fib Deepens Hopes for Primary Prevention from Heartwire — a professional news service of WebMD February 27, 2009 (Framingham, Massachusetts) http://www.medscape.com/viewarticle/588887
- ^ Поликлиническая терапия. Учебник. — Под ред. проф. И. Л. Давыдкина, проф. Ю. В. Щукина. — М.: ГЭОТАР-Медиа, 2013. — 688c. — ISBN 978-5-9704-2396-7 — C. 114-115.
Silent stroke
With regards to silent stroke, this needs discussing in context. Kalantarian S, Ay H, Gollub RL, Lee H, Retzepi K, Mansour M, Ruskin JN (4 Nov 2014). "Association Between Atrial Fibrillation and Silent Cerebral Infarctions: A Systematic Review and Meta-analysis". Ann Intern Med. 161 (9): 650–8. doi:10.7326/M14-0538. PMID 25364886.{{cite journal}}: CS1 maint: multiple names: authors list (link)
Currently the "pathophysiology" section does not mention how atrial thrombi lead to stroke. This needs covering (e.g. the role of the LA appendage). JFW | T@lk 11:26, 7 November 2014 (UTC)
Missed key source?
AHA/ACC/HRS issued a new guideline in March, but I don't think anyone noticed.
- doi:10.1161/CIR.0000000000000040 - Executive summary
- doi:10.1161/CIR.0000000000000041 - Full guideline
Could be used for updating. JFW | T@lk 20:04, 2 December 2014 (UTC)
Stroke prevention review
In JAMA doi:10.1001/jama.2015.4369 JFW | T@lk 14:53, 20 May 2015 (UTC)
- And more: doi:10.1001/jama.2015.3088, doi:10.1001/jama.2015.7505 JFW | T@lk 13:26, 22 July 2015 (UTC)
Review of stroke prevention
Lancet review on stroke prevention, particularly the trickier areas such as comorbidity and renal impairment doi:10.1016/S0140-6736(15)60245-8 JFW | T@lk 14:41, 17 July 2015 (UTC)
- And now a "Series" from the Lancet here. JFW | T@lk 22:42, 22 August 2016 (UTC)
External links modified
Hello fellow Wikipedians,
I have just modified one external link on Atrial fibrillation. Please take a moment to review my edit. If you have any questions, or need the bot to ignore the links, or the page altogether, please visit this simple FaQ for additional information. I made the following changes:
- Added archive https://web.archive.org/web/20160305114229/http://jaoa.org/content/112/9_suppl_2/es2.long to http://www.jaoa.org/content/112/9_suppl_2/eS2.long
When you have finished reviewing my changes, please set the checked parameter below to true or failed to let others know (documentation at {{Sourcecheck}}).
This message was posted before February 2018. After February 2018, "External links modified" talk page sections are no longer generated or monitored by InternetArchiveBot. No special action is required regarding these talk page notices, other than regular verification using the archive tool instructions below. Editors have permission to delete these "External links modified" talk page sections if they want to de-clutter talk pages, but see the RfC before doing mass systematic removals. This message is updated dynamically through the template {{source check}} (last update: 5 June 2024).
- If you have discovered URLs which were erroneously considered dead by the bot, you can report them with this tool.
- If you found an error with any archives or the URLs themselves, you can fix them with this tool.
Cheers.—InternetArchiveBot (Report bug) 01:26, 21 October 2016 (UTC)
Requesting an assessment of Anticoagulants within Management Section
Dear Editors, I am posting here regarding a paragraph that appears on the atrial fibrillation Wikipedia page to highlight some additional references that may provide further context about the use of NOACs for stroke prevention in patients with atrial fibrillation. The paragraph I am referring to is: For those with non-valvular atrial fibrillation, the NOACs (rivaroxaban, dabigatran, apixaban) are neither superior nor worse than warfarin in preventing non-hemorrhagic stroke and systemic embolic events.[44][45] They have a lower risk of intracranial bleeding compared to warfarin; however, dabigatran is associated with a higher risk of gastrointestinal bleeding.[44][45] There are two points to note and I politely request that you consider updating the page to provide a full and balanced picture. 1. The paragraph notes that rivaroxaban, dabigatran and apixaban are: ‘neither superior nor worse than warfarin in preventing non-hemorrhagic stroke and systemic embolism.’ Based on a paper by CT Ruff and colleagues (full reference, Ruff CT et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383:955-62), you may wish to consider updating to acknowledge that the NOACs ‘significantly reduce’ stroke and systemic embolism events, rather than being ‘neither superior not worse’. Furthermore, you may also want to include edoxaban in the list of NOACs? 2. Secondly, you might also consider updating the text around the risk of GI bleeding as differences in rates of GI bleeding have been seen between the NOAC regimens. Compared to warfarin the risk of GI bleeding was increased: - with the standard dose of dabigatran (150 mg twice daily) in patients >75 years of age. No increase in GI bleeding versus warfarin was seen in younger patients treated with dabigatran 150 mg twice daily, nor any age groups treated with the reduced dose of dabigatran 110 mg twice daily [Connolly, Connolly, Eikelboom] - with both doses of rivaroxaban (20 mg once daily or 15 mg once daily) in all age groups [Patel, Sherwood, Halperin] - with edoxaban in patients treated with the high dose regimen (60 mg once daily as the standard dose or 30 mg once daily in patients with certain risk factors). No increase in GI bleeding versus warfarin was seen with the low dose regimen of edoxaban (30 mg once daily as the standard dose or 15 mg once daily in patients with certain risk factors) [Giugliano]. Please note that the low dose regimen of edoxaban is only approved in Japan.
The reference list to support the above clinical findings are: a. Connolly SJ et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 2009;361:1139–5 b. Connolly SJ, Ezekowitz MD, Yusuf S, Reilly PA, Wallentin L. Newly identified events in the RE-LY trial. N Engl J Med. 2010;363(19):1875-6. c. Eikelboom JW et al. Risk of bleeding with 2 doses of dabigatran compared with warfarin in older and younger patients with atrial fibrillation: an analysis of the randomized evaluation of long-term anticoagulant therapy (RE-LY) trial. Circulation 2011 31;123(21):2363–72 d. Patel MR et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011 Sep 8;365(10):883–91 e. Sherwood MW, Nessel CC, Hellkamp AS, Mahaffey KW, Piccini JP, Suh EY et al. Gastrointestinal Bleeding in Patients With Atrial Fibrillation Treated With Rivaroxaban or Warfarin: ROCKET AF Trial. J Am Coll Cardiol. 2015 Dec 1;66(21):2271–81 f. Halperin J.L. et al. Efficacy and Safety of Rivaroxaban Compared With Warfarin Among Elderly Patients With Nonvalvular Atrial Fibrillation in the Rivaroxaban Once Daily, Oral, Direct Factor Xa Inhibition Compared With Vitamin K Antagonism for Prevention of Stroke and Embolism Trial in Atrial Fibrillation (ROCKET AF). Circulation 2014;130(2):138–46 g. Giugliano RP et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med 2013;369:2093–104
Please let me know if any additional information or resources are needed. Do not hesitate to contact me on my Talk Page with questions. Many thanks — Preceding unsigned comment added by J craig.hunter (talk • contribs) 13:27, 15 December 2016 (UTC)
Most episodes
From the lead,
- "Most episodes have no symptoms.[1]"
The above statement in the lead is contradicted by the source in the previous sentence of the lead [2].
References
- ^ Munger, TM; Wu, LQ; Shen, WK (January 2014). "Atrial fibrillation". Journal of biomedical research. 28 (1): 1–17. doi:10.7555/JBR.28.20130191. PMC 3904170. PMID 24474959.
- ^ Zoni-Berisso, M; Lercari, F; Carazza, T; Domenicucci, S (2014). "Epidemiology of atrial fibrillation: European perspective". Clinical epidemiology. 6: 213–20. doi:10.2147/CLEP.S47385. PMC 4064952. PMID 24966695.
{{cite journal}}: CS1 maint: unflagged free DOI (link)
--Bob K31416 (talk) 09:40, 16 August 2017 (UTC)
American Heart Association – "Sometimes people with AFib have no symptoms and their condition is only detectable upon physical examination. Still, others may experience one or more of the following symptoms: ..."
American College of Cardiology – "You might feel short of breath, dizzy and overly tired, although not everyone has these symptoms." --Bob K31416 (talk) 02:39, 17 August 2017 (UTC)
Infobox image and caption
In the info box, the image and its caption don't clearly describe afib. The RR intervals of the ECG look approximately equal and the caption would be probably read to mean that the atria are fibrillating at about 150 BPM. Also, no mention is made of the missing P wave. --Bob K31416 (talk) 09:57, 16 August 2017 (UTC)
- Clarified Doc James (talk · contribs · email) 21:45, 16 August 2017 (UTC)
Per these details in the lead
"Most people with atrial fibrillation are at high risk of stroke and require treatment with anti-clotting medications such as a novel oral anticoagulant (NOAC) (e.g., apixaban) or warfarin to reduce this risk.[1] People with atrial fibrillation and moderate risk for stroke should usually receive a NOAC or warfarin but aspirin may be considered.[1] Individuals with atrial fibrillation who are at low risk for stroke may not require anti-clotting medications or aspirin.[1]"
A couple of things:
- They do not require treatment but it is often recommended
- One must also keep in mind "Stroke prophylaxis in AF must balance a patient's thromboembolic risk with their bleeding risk."
I think these details fit better in the body than the lead and it is better to keep the lead simpler. Thus moved. Doc James (talk · contribs · email) 22:43, 23 December 2017 (UTC)
Text
First sentence
- "Most people with atrial fibrillation are at high risk of stroke and require treatment with anti-clotting medications" such as a novel oral anticoagulant (NOAC) (e.g., apixaban) or warfarin to reduce this risk.[1]
Not seeing were the ref says most people with afib are at high risk.
Also not seeing were it says "require"
Doc James (talk · contribs · email) 00:09, 25 December 2017 (UTC)
- Doc James, the current version is inaccurate and only reflects the AHA/ACC guidelines. The remainder of the guidelines cited do not recommend aspirin as a treatment (some even directly recommend against its use). If you want to change the "high-risk" part and rephrase it, that's fine, but the fact remains that various guidelines say that most people with atrial fibrillation need anticoagulation (and thus are at high risk of stroke from their atrial fibrillation-otherwise, why are we anticoagulating them if they're not at high risk?). The word require was a word choice selection and didn't come directly from a source. It strikes me as a bit nitpicky to focus on that. I have no objection to saying "recommend" or something similar to that but it is the standard of care and aspirin is not. TylerDurden8823 (talk) 06:25, 25 December 2017 (UTC)
- Also, here is a direct quote from the 2016 ESC guidelines verbatim: "The net clinical benefit is almost universal, with the exception of patients at very low stroke risk, and OAC should therefore be used in most patients with AF (Figure 8). Despite this evidence, underuse or premature termination of OAC therapy is still common. "TylerDurden8823 (talk) 06:25, 25 December 2017 (UTC)
- TylerDurden8823 How is this inaccurate "For those at low risk of stroke either nothing, aspirin, or anti-clotting medications such as warfarin or a direct oral anticoagulant may be recommended."? These are all potential recommendations for those at low risk. Doc James (talk · contribs · email) 07:05, 25 December 2017 (UTC)
- Doc James, I think it's too oversimplified. It sounds like those are all equally valid options even though the aspirin is considered a minority opinion but it feels as if it's being given equivalent weight. I don't think it should be. There's tons of precedent where we don't give the minority view equal weight. TylerDurden8823 (talk) 07:08, 25 December 2017 (UTC)
- Some recommend nothing for those with a CHA2DS2-VASc score of zero including the 2016 ESC guidelines. They give this a level of evidence of IIIB. Not exactly a strong endorsement.
- Some recommend ASA "For patients with nonvalvular AF and a CHA2DS2-VASc score of 1, no antithrombotic therapy or treatment with an oral anticoagulant or aspirin may be considered" giving this a level of evidence of IIb (level C)[8] Also not a strong recommendation.
- None of the options are well supported. Doc James (talk · contribs · email) 07:28, 25 December 2017 (UTC)
- Doc James, many guidelines recommend nothing for CHADS2VASC of 0. That's not the part that feels oversimplified but for CHADS2VASC 1. Where exactly are you drawing the line for "low-risk" in this statement? CHADS2VASC 0 or 1? TylerDurden8823 (talk) 07:33, 25 December 2017 (UTC)
- This is what the body of the article is for. Running through the specific recommendation for each CHADS2VASC score. Low risk typically groups 0 and 1. And there are three recommended option within this grouping. Doc James (talk · contribs · email) 07:59, 25 December 2017 (UTC)
- Doc James, many guidelines recommend nothing for CHADS2VASC of 0. That's not the part that feels oversimplified but for CHADS2VASC 1. Where exactly are you drawing the line for "low-risk" in this statement? CHADS2VASC 0 or 1? TylerDurden8823 (talk) 07:33, 25 December 2017 (UTC)
- Doc James, I think it's too oversimplified. It sounds like those are all equally valid options even though the aspirin is considered a minority opinion but it feels as if it's being given equivalent weight. I don't think it should be. There's tons of precedent where we don't give the minority view equal weight. TylerDurden8823 (talk) 07:08, 25 December 2017 (UTC)
- TylerDurden8823 How is this inaccurate "For those at low risk of stroke either nothing, aspirin, or anti-clotting medications such as warfarin or a direct oral anticoagulant may be recommended."? These are all potential recommendations for those at low risk. Doc James (talk · contribs · email) 07:05, 25 December 2017 (UTC)
- Also, here is a direct quote from the 2016 ESC guidelines verbatim: "The net clinical benefit is almost universal, with the exception of patients at very low stroke risk, and OAC should therefore be used in most patients with AF (Figure 8). Despite this evidence, underuse or premature termination of OAC therapy is still common. "TylerDurden8823 (talk) 06:25, 25 December 2017 (UTC)
Sentence two
"People with atrial fibrillation and moderate risk for stroke should usually receive a NOAC or warfarin but aspirin may be considered."[1]
Sure but belongs in the body.
Doc James (talk · contribs · email) 00:09, 25 December 2017 (UTC)
- I disagree, I think this should be briefly mentioned in the lead as well. This is a very long article and anticoagulation deserves more discussion in the lead since it's a crucial component of atrial fibrillation management. Aspirin misuse (as mentioned in the body) is highly prevalent and I think such information would benefit primary care physicians and a general lay audience (many people who read this article may be currently treated with aspirin but actually need anticoagulation). A bit more summary belongs in the lead than is currently there. TylerDurden8823 (talk) 06:25, 25 December 2017 (UTC)
- We now say "For those at more than low risk an anti-clotting medication is typically recommended." I think that covers it well. Doc James (talk · contribs · email) 07:11, 25 December 2017 (UTC)
- I suppose that's fine for simplified language in the lead which can be expanded on more in the body. TylerDurden8823 (talk) 07:13, 25 December 2017 (UTC)
- We now say "For those at more than low risk an anti-clotting medication is typically recommended." I think that covers it well. Doc James (talk · contribs · email) 07:11, 25 December 2017 (UTC)
Sentence three
"Aspirin is generally not considered to be a safe or effective method for reducing the risk of strokes from atrial fibrillation and has not been well-validated for this use."[1][2]
Ref also says "For those with a CHA2DS2-VASc score of 1, OACs, aspirin, or no antithrombotic treatment can be chosen, depending on risk factors and patient values and preferences."
But than it also says "Aspirin alone should not be offered for stroke prevention in atrial fibrillation"
Doc James (talk · contribs · email) 00:09, 25 December 2017 (UTC)
- The mayo ref also says "Despite not having been studied in a low-risk population, because of its low risk, aspirin is an option for patients with a CHA2DS2-VASc score of 1 or less."
- Aspirin is generally safe, the issue is more that among those at risk of stroke it does not decrease stroke as much / aswell as anticoagulants. Anyway it is controversial. Some still recommend aspirin as a possibility in low risk people. It can be fleshed out in the body. Doc James (talk · contribs · email) 00:22, 25 December 2017 (UTC)
- Okay, here is what the Freedman article says verbatim:
- Aspirin is generally safe, the issue is more that among those at risk of stroke it does not decrease stroke as much / aswell as anticoagulants. Anyway it is controversial. Some still recommend aspirin as a possibility in low risk people. It can be fleshed out in the body. Doc James (talk · contribs · email) 00:22, 25 December 2017 (UTC)
"Aspirin is still widely misused for primary or even secondary stroke prevention in a quarter to a third of patients with atrial fibrillation who are eligible for OACs,24,25 presumably because of misperception of efficacy and safety for stroke prevention in atrial fibrillation, which is likely to contribute to continuing underuse of anticoagulants.26 Aspirin is neither effective nor safe as thromboprophylaxis for atrial fibrillation,26 even possibly increasing stroke risk in elderly patients,27 and has largely been removed from guidelines.19,28,29" The consequence of aspirin misuse is evident in stroke registries (appendix pp 3, 4, 6), with a high proportion of atrial-fibrillation-related strokes occurring in patients treated only with aspirin, despite a CHADS2 or CHA2DS2-VASc score of at least 2 (appendix pp 3, 4). Replacing aspirin with OACs, and prescribing OACs for the 20% of high-risk patients with known atrial fibrillation who receive no OAC treatment (appendix p 6) constitutes a simple solution to reduce the atrial fibrillation stroke burden, provided effective measures to close this evidence–treatment gap are implemented.
Then, the Freedman article says this: "The evidence is compelling that even a single stroke risk factor confers an excess risk of thromboembolism and mortality (figure 3),60–62 with a positive net clinical benefit for OAC treatment compared with aspirin or no antithrombotic treatment for such patients.60,63"
- James, for the passage you cited above: ""For those with a CHA2DS2-VASc score of 1, OACs, aspirin, or no antithrombotic treatment can be chosen, depending on risk factors and patient values and preferences", this is not in the author's voice but is a reiteration of what the AHA/ACC guidelines say (but not the other guidelines and reflects a minority opinion). After rereading this passage, I can see how this might have misled you to believe this was the authors' message, but it's not.
Aspirin's bleeding risk is comparable to that of warfarin and the NOACs (I added references specifying this which directly state this including Freedman's article and the 2016 ESC guidelines). It is not controversial at all and is clearly agreed upon in the literature. The vast majority of the guidelines agree that aspirin is not recommended even for CHADS2VASC1 (I added three from ESC, CCS, and NICE; I mentioned very select circumstances (e.g., CHADSVASC 0-1 if they have comorbid CAD but that's not really for stroke prophylaxis)). I imagine the next ACC/AHA guideline will do away with aspirin too once it's written but only time will tell. The Morin ref supports this as well: "For patients with moderate risk (CHA2DS2-VASc score, 1), the full gambit of possible prophylactic approaches (OAC, aspirin, or even no therapy) may all be considered, though expert opinion leans toward full anticoagulation".
The Morin article also says a few other things supporting this: "For patients at high risk as well as in select patients with moderate risk, OAC therapy is advised for the reduction of stroke and systemic embolism." (that's most patients but if you require a reference that explicitly says "most", I'm sure I can find some). The article also says:"Early trials examining stroke prevention in AF focused on warfarin and antiplatelet agents. Aspirin alone has exhibited essentially no meaningful effect on stroke reduction, with only the Stroke Prevention in Atrial Fibrillation (SPAF) trial reporting any significant benefit.161,162" Yes, it's technically considered an option (in the AHA guidelines) but this is really a minority opinion and most experts agree that anticoagulation is the treatment of choice for CHADSVASC2 score of 1 (unless the point is only due to female sex as mentioned in the Andrade 2017 review). TylerDurden8823 (talk) 06:25, 25 December 2017 (UTC)
- Disagree. The "AHA/ACC guidelines" is not a "minority opinion".
- It is from 2014. Yes if it removes ASA in the next guideline so should we. Doc James (talk · contribs · email) 07:12, 25 December 2017 (UTC)
- How is 1/4 guidelines not a minority opinion when the other three mentioned all unanimously disagree on that particular point? I agree that once the ACC/AHA removes ASA from the guidelines we'll reflect that. TylerDurden8823 (talk) 07:16, 25 December 2017 (UTC)
- The AHA/ACC is simple not a "minority opinion". It is a major opinion. Doc James (talk · contribs · email) 07:22, 25 December 2017 (UTC)
- Yes, it's a major opinion in terms of significance (minority is not meant to reduce the significance of the AHA/ACC's opinion) but remains the minority opinion in terms of simple math (1 out of 4 guidelines identified so far). The ACC/AHA are not more important (and are not to be given more weight) than the ESC, CCS, and/or NHS (and certainly not when all of them agree in contrast to the AHA's statement). TylerDurden8823 (talk) 07:29, 25 December 2017 (UTC)
- I disagree that these sorts of disputes are or should solved by "simple math". ACC and AHA count as two organisations so we are at 3:2 at best. Doc James (talk · contribs · email) 07:33, 25 December 2017 (UTC)
- Disagree, it's a unified guideline and therefore one position statement. I think more eyes are needed here. Will raise this at Wikiproject Medicine. Currently looking to see if other guidelines address this too. Again, ACC/AHA is not more important than the other guideline groups. Three guideline position statements are definitely the majority opinion over one guideline statement (not to mention they're also more updated). TylerDurden8823 (talk) 07:38, 25 December 2017 (UTC)
- The ACCP and Asia Pacific Heart Rhythm Society guidelines also state CHADS2VASC 1 should be on oral anticoagulants instead of aspirin. That's five guidelines now in consensus against the ACC/AHA's recommendation on CHADS2VASC 1.
- One good guideline is enough to include ASA as a potentially recommended option. Sure we can get further opinions. Doc James (talk · contribs · email) 07:55, 25 December 2017 (UTC)
- The ACCP and Asia Pacific Heart Rhythm Society guidelines also state CHADS2VASC 1 should be on oral anticoagulants instead of aspirin. That's five guidelines now in consensus against the ACC/AHA's recommendation on CHADS2VASC 1.
- Disagree, it's a unified guideline and therefore one position statement. I think more eyes are needed here. Will raise this at Wikiproject Medicine. Currently looking to see if other guidelines address this too. Again, ACC/AHA is not more important than the other guideline groups. Three guideline position statements are definitely the majority opinion over one guideline statement (not to mention they're also more updated). TylerDurden8823 (talk) 07:38, 25 December 2017 (UTC)
- I disagree that these sorts of disputes are or should solved by "simple math". ACC and AHA count as two organisations so we are at 3:2 at best. Doc James (talk · contribs · email) 07:33, 25 December 2017 (UTC)
- Yes, it's a major opinion in terms of significance (minority is not meant to reduce the significance of the AHA/ACC's opinion) but remains the minority opinion in terms of simple math (1 out of 4 guidelines identified so far). The ACC/AHA are not more important (and are not to be given more weight) than the ESC, CCS, and/or NHS (and certainly not when all of them agree in contrast to the AHA's statement). TylerDurden8823 (talk) 07:29, 25 December 2017 (UTC)
- The AHA/ACC is simple not a "minority opinion". It is a major opinion. Doc James (talk · contribs · email) 07:22, 25 December 2017 (UTC)
- How is 1/4 guidelines not a minority opinion when the other three mentioned all unanimously disagree on that particular point? I agree that once the ACC/AHA removes ASA from the guidelines we'll reflect that. TylerDurden8823 (talk) 07:16, 25 December 2017 (UTC)
Canadian Guidelines say "It recommends OAC for most patients ≥65 years and for younger patients with a CHADS2 score≥1; aspirin (ASA) for patients<65 years with CHADS2 score=0 with arterial vascular disease (coronary, aortic, or peripheral); and no antithrombotic therapy for patients <65 years with a CHADS2 score=0 and no arterial vascular disease."[9]
- It remains a minority opinion against seven other guidelines from good guidelines. ESC, CCS, ACCP, JCS, etc all put out good guidelines too. I think you're placing far too much weight on the ACC/AHA's single guideline against overwhelming international consensus. TylerDurden8823 (talk) 08:34, 25 December 2017 (UTC)
2016 Guideline says "In general, oral anticoagulation (OAC) therapy is recommended for all patients with AF except those younger than 65 years of age with a Congestive Heart Failure, Hypertension, Age, Diabetes, Stroke/Transient Ischemic Attack (CHADS2) score of 0. In the latter group, aspirin (acetylsalicylic acid; ASA) is recommended in patients with CAD/vascular disease, and there is no indication for antithrombotic treatment in the absence of CAD/vascular disease."[10]Doc James (talk · contribs · email) 08:01, 25 December 2017 (UTC)
- It's now seven guidelines that do not recommend aspirin for CHADS2VASC 1 (many of them outright state they do not recommend aspirin monotherapy whatsoever). The AHA/ACC guideline is clearly the outlier. I already acknowledged the point you raised immediately above in an earlier edit summary that ASA has a role for CHADS2VASC 0 if there's comorbid CAD/PAD (but again, that's not really meant for stroke prophylaxis from Afib). I think you may be getting confused about which point is being debated here (recommendations for CHADS2VASC 1 (except when female sex is the only risk factor rather than true stroke risk factors as discussed in numerous guidelines), not 0). TylerDurden8823 (talk) 08:32, 25 December 2017 (UTC)
- And another guideline that says ASA may be used as well "Antiplatelet drugs may be considered for patients who cannot use oral anticoagulants. (Level of Evidence: C)"[11]
- So 6 guidelines to 4. Meh. Also many are not so cut and dried. Doc James (talk · contribs · email) 08:39, 25 December 2017 (UTC)
- James, that's incorrect. Meh? How did you arrive at four guidelines? It's 7 to 1 (ACC/AHA is one unified guideline). The JCS guideline clearly states (with a level 1A recommendation) that OAC is to be offered for CHADS2VASC 1. Period. It makes sense that antiplatelets would be tried if OAC were intolerable for someone but that's hardly recommending it. I think it's important to remember that the original statement was that the consensus is that oral anticoagulation is preferred over aspirin for CHADS2VASC 1. The JCS guideline you're citing is still consistent with that statement. Direct quote from the document you're citing: "Anticoagulation therapy with dabigatran (Level of Evidence: B) or apixaban (Level of Evidence: A) should be performed in intermediate-risk patients with a CHADS2 score of 1." TylerDurden8823 (talk) 08:47, 25 December 2017 (UTC)
- Tyler we are talking about options for low risk patients which also includes "0" patients. The Chest Physicians Guideline says "For patients with nonrheumatic AF, including those with paroxysmal AF, who are (1) at low risk of stroke (eg, CHADS2 [congestive heart failure, hypertension, age ≥ 75 years, diabetes mellitus, prior stroke or transient ischemic attack] score of 0), we suggest no therapy rather than antithrombotic therapy, and for patients choosing antithrombotic therapy, we suggest aspirin rather than oral anticoagulation or combination therapy with aspirin and clopidogrel"[12] So it is there as an option aswell.
- Anyway I think the wording now in the lead reflects the literature. In low risk people either nothing, ASA, and anticogulants are recommended. In those at more than low risk typically anticogulants are recommended. Doc James (talk · contribs · email) 08:54, 25 December 2017 (UTC)
- James, that's incorrect. Meh? How did you arrive at four guidelines? It's 7 to 1 (ACC/AHA is one unified guideline). The JCS guideline clearly states (with a level 1A recommendation) that OAC is to be offered for CHADS2VASC 1. Period. It makes sense that antiplatelets would be tried if OAC were intolerable for someone but that's hardly recommending it. I think it's important to remember that the original statement was that the consensus is that oral anticoagulation is preferred over aspirin for CHADS2VASC 1. The JCS guideline you're citing is still consistent with that statement. Direct quote from the document you're citing: "Anticoagulation therapy with dabigatran (Level of Evidence: B) or apixaban (Level of Evidence: A) should be performed in intermediate-risk patients with a CHADS2 score of 1." TylerDurden8823 (talk) 08:47, 25 December 2017 (UTC)
- We should clarify cutoffs of CHADS2VASC/CHADS2 =0 as low-risk, CHADS2VASC/CHADS2=1 intermediate-risk, and CHADS2/CHADS2VASC 2+ as high-risk. Even we weren't on the same page about that. Imagine how confusing it would be for patients. TylerDurden8823 (talk) 09:03, 25 December 2017 (UTC)
- Ref also says "For those with a CHA2DS2-VASc score of 1, OACs, aspirin, or no antithrombotic treatment can be chosen, depending on risk factors and patient values and preferences."
- But than it also says "Aspirin alone should not be offered for stroke prevention in atrial fibrillation"
- I think I have provided substantial evidence that aspirin is widely regarded (by many guidelines and most experts including high-quality reviews of these guidelines) as an ineffective and unvalidated treatment to reduce the risk of stroke in atrial fibrillation. Oral anticoagulation is widely preferred over aspirin for CHADS/CHADS2VASC1. You said aspirin is generally safe and reasonable for those with high bleeding risk but the evidence disagrees with this statement (again, bleeding risk is comparable-we outright state this in the article). I addressed your earlier point about the Freedman article that this was merely a reiteration of the ACC/AHA joint guidelines and not the author's own opinion (but the last sentence you quoted is-that aspirin alone should not be offered for stroke prevention in atrial fibrillation). TylerDurden8823 (talk) 09:01, 25 December 2017 (UTC)
- James, you're really beginning to frustrate me because your refusals indicate that you are not reading all of the content I have put here. Again, you refer to CHADS2VASC 1 as low-risk; however, this quote clearly states this is incorrect: ""Anticoagulation therapy with dabigatran (Level of Evidence: B) or apixaban (Level of Evidence: A) should be performed in intermediate-risk patients with a CHADS2 score of 1." The changes I made were absolutely fine. I do not think you have sufficient presented your case. TylerDurden8823 (talk) 09:12, 25 December 2017 (UTC)
- IMO we should not be described CHA2DS2-VASc score in the lead. Will work on drafting a RfC Doc James (talk · contribs · email) 09:14, 25 December 2017 (UTC)
- Please explain why not because the way it's written now conflates low and intermediate risk and numerous articles clearly state this is an important distinction. Also, please be sure to respond in full to the points made above. (it comes across as those points being ignored if you don't address them). TylerDurden8823 (talk) 09:19, 25 December 2017 (UTC)
- User:TylerDurden8823 I am working on providing evidence for the current version as I set up the RfC. Some (specifically NICE) also call a 1 among women low risk and include that group among those needing no treatment. Doc James (talk · contribs · email) 09:32, 25 December 2017 (UTC)
- Yes aspirin is not typically a preferred choice. Yet it is still presented as an option for some at lower risk in certain guidelines. Doc James (talk · contribs · email) 09:40, 25 December 2017 (UTC)
- Sigh, I addressed this multiple times above James. This tells me you did not read my earlier comments carefully. I already clearly stated that CHADS2VASC 1 (if the only point was for female sex) is not a clear indication for anticoagulation, it's really for CHADS2VASC 1 with a specific stroke risk factor. If you really insist on qualifying that (even though that introduces even more nuance in the lead), then that's fine. TylerDurden8823 (talk) 09:41, 25 December 2017 (UTC)
- And yet you added this "For those at intermediate (CHADS2VASC 1) ... anti-clotting medication such as warfarin or a novel oral anticoagulant (e.g., apixaban) is typically recommended." Even though 40% of people with afib are women.
- User:TylerDurden8823 let me know if the version 2 is the one you wish to propose in a RfC? Doc James (talk · contribs · email) 09:46, 25 December 2017 (UTC)
- James, please see below. Okay, once again, I've already said (multiple times now) that CHADS2VASC 1 for men/2 for women is acceptable since 1 point is assigned for female sex but anticoag isn't recommended for women with CHADS2VASC 1 only for female sex (note: CHADS2 system does not include female sex as a risk factor). Please, please read my earlier comments. I've addressed this multiple times in edit summaries and my comments. It's very frustrating repeating myself. TylerDurden8823 (talk) 10:11, 25 December 2017 (UTC)
- Yes we all agree that "anticoag isn't recommended for women with CHADS2VASC 1 only for female sex" and yes I know you have stated that a bunch. And yes I have read it a bunch and agree entirely with you on this point. Women with a score of 1 are included in "lower risk" / "low risk"
- What you added to the lead does not include that nuance that you have brought up multiple times and which I have read multiple times and which I have agreed with multiple times and have absolutely no problem with. IMO this is why it is overly complicated to introduce the CHADS2VASC scoring system in the lead as one than need to add the exception that you mention.
- We also both agree that anti coagulation is generally the treatment for anything above low risk. We may disagree slightly on whether or not ASA should be listed as an option for those with low risk? But you included it as an option in your version so maybe we do not even disagree on that. Doc James (talk · contribs · email) 10:19, 25 December 2017 (UTC)
- I put that there temporarily. I still think the RFC is necessary to discuss better definitions of low, intermediate, and high risk. I don't agree that discussing CHADS2 or CHADS2VASC has to be complicated. I think with a bit of work it can be introduced simply. It was not at all clear from your earlier statements that you agreed that anticoagulation is the preferred therapy for anything over low risk since I kept talking about CHADS2VASC 1 and you intermittently mentioned CHADS2VASC 0 (again, you defined CHADS2VASC 1 as low risk but didn't mention the female caveat earlier, you just used it as a blanket statement, which is false for men). It's possible there was some communication breakdown. I still think a brief mention that aspirin is not a well-validated therapy in the lead is appropriate and well-supported by the evidence. Aspirin's role in atrial fibrillation is minimal and guidelines are increasingly doing away with it (and most likely will continue to do so; non-guideline reviews such as the Mayo article and Andrade review also discuss this). TylerDurden8823 (talk) 10:30, 25 December 2017 (UTC)
- I think the main disagreement we are having is over how complicated the language should be. I thought "For those at more than low risk an anti-clotting medication is typically recommended" is fairly clear.
- IMO those at moderate risk should also generally be anti-coagulated and thought you User:TylerDurden8823 believed the same. I thus find this change strange.[13] Doc James (talk · contribs · email) 10:36, 25 December 2017 (UTC)
- I put that there temporarily. I still think the RFC is necessary to discuss better definitions of low, intermediate, and high risk. I don't agree that discussing CHADS2 or CHADS2VASC has to be complicated. I think with a bit of work it can be introduced simply. It was not at all clear from your earlier statements that you agreed that anticoagulation is the preferred therapy for anything over low risk since I kept talking about CHADS2VASC 1 and you intermittently mentioned CHADS2VASC 0 (again, you defined CHADS2VASC 1 as low risk but didn't mention the female caveat earlier, you just used it as a blanket statement, which is false for men). It's possible there was some communication breakdown. I still think a brief mention that aspirin is not a well-validated therapy in the lead is appropriate and well-supported by the evidence. Aspirin's role in atrial fibrillation is minimal and guidelines are increasingly doing away with it (and most likely will continue to do so; non-guideline reviews such as the Mayo article and Andrade review also discuss this). TylerDurden8823 (talk) 10:30, 25 December 2017 (UTC)
- James, please see below. Okay, once again, I've already said (multiple times now) that CHADS2VASC 1 for men/2 for women is acceptable since 1 point is assigned for female sex but anticoag isn't recommended for women with CHADS2VASC 1 only for female sex (note: CHADS2 system does not include female sex as a risk factor). Please, please read my earlier comments. I've addressed this multiple times in edit summaries and my comments. It's very frustrating repeating myself. TylerDurden8823 (talk) 10:11, 25 December 2017 (UTC)
- User:TylerDurden8823 I am working on providing evidence for the current version as I set up the RfC. Some (specifically NICE) also call a 1 among women low risk and include that group among those needing no treatment. Doc James (talk · contribs · email) 09:32, 25 December 2017 (UTC)
- Please explain why not because the way it's written now conflates low and intermediate risk and numerous articles clearly state this is an important distinction. Also, please be sure to respond in full to the points made above. (it comes across as those points being ignored if you don't address them). TylerDurden8823 (talk) 09:19, 25 December 2017 (UTC)
- IMO we should not be described CHA2DS2-VASc score in the lead. Will work on drafting a RfC Doc James (talk · contribs · email) 09:14, 25 December 2017 (UTC)
Sentence four
"Individuals with atrial fibrillation who are at low risk for stroke may not require anti-clotting medications or aspirin."[1]
Once again belongs in the body IMO. Doc James (talk · contribs · email) 23:55, 24 December 2017 (UTC)
- Again, I disagree. I believe this deserves brief mention in the lead as well for aforementioned reasons. TylerDurden8823 (talk) 06:25, 25 December 2017 (UTC)
- It is now summarized within "For those at low risk of stroke either nothing, aspirin, or anti-clotting medications such as warfarin or a direct oral anticoagulant may be recommended." Doc James (talk · contribs · email) 07:12, 25 December 2017 (UTC)
- Again, I disagree. I believe this deserves brief mention in the lead as well for aforementioned reasons. TylerDurden8823 (talk) 06:25, 25 December 2017 (UTC)
References
- ^ a b c d e f g h Morin, DP; Bernard, ML; Madias, C; Rogers, PA; Thihalolipavan, S; Estes 3rd, NA (December 2016). "The State of the Art: Atrial Fibrillation Epidemiology, Prevention, and Treatment". Mayo Clinic Proceedings. 91 (12): 1778-1810. doi:10.1016/j.mayocp.2016.08.022. PMID 27825618.
{{cite journal}}: CS1 maint: numeric names: authors list (link) - ^ a b Freedman, B; Potpara, TS; Lip, GY (August 2016). "Stroke prevention in atrial fibrillation". The Lancet (Review). 388 (10046): 806-17. doi:10.1016/S0140-6736(16)31257-0. PMID 27560276.
RfC
- The following discussion is an archived record of a request for comment. Please do not modify it. No further edits should be made to this discussion. A summary of the conclusions reached follows.
Which of these sentences should go as a summary of treatment recommendations in the lead of this article? Doc James (talk · contribs · email) 23:50, 25 December 2017 (UTC)
Version 1
For those at lower risk of stroke either nothing, aspirin, or an anti-clotting medications may be recommended.[1] Anti-clotting medications include warfarin and direct oral anticoagulants.[1] For those at more than low risk an anti-clotting medication is typically recommended.[1]
- Reasoning
1 a) Quote = Refering to the ACC/AHA guidelines "Low risk are those with a CHA2DS2-VASc score of 0, for whom no antithrombotic treatment should be considered. For those with a CHA2DS2-VASc score of 1, OACs, aspirin, or no antithrombotic treatment can be chosen, depending on risk factors and patient values and preferences."[1] This is recommended one of three options for lower risk (0 or 1).
1 b) "The 2014 NICE guidelines and European Society of Cardiology guidelines recommend that the initial step should be to identify low-risk patients (CHA2DS2-VASc score 0 in males, 1 in females) who do not need antithrombotic treatment."[1] This bit of text is also including a score of 1 among low risk not needing specific treatment and thus one more reason not to bring in the exact scores until later. It is also why version 2 below IMO is incorrect.
2) Some such as Uptodate also say anticoagulation is an option for those with a CHA2DS2-VASc score of 0. "For patients with a CHA2DS2-VASc of 0 or 1 in females, we suggest no anticoagulant therapy (Grade 2C). Patients who are particularly stroke averse and who are at low bleeding risk may reasonably choose anticoagulation."[14]
3) With respect to keeping the lead easier to understand I do not think we need to introduce the CHADS2VASC scoring system in the lead. Doing so accurately would involve a fair bit of text and IMO is best done in the body of the article were details can be provided with appropriate nuance.
4) Uptodate also says "The benefit to risk ratio from oral anticoagulation in patients at very low (CHA2DS2-VASc score of 0) and low risk (CHA2DS2-VASc score of 1) has not been well studied"[15] The terminology of what falls into each group is not consistent.
References
Version 2
For those at low risk of stroke (CHADS2VASC 0) either nothing or aspirin are typically recommended.[1] For those at intermediate (CHADS2VASC 1) or high risk of stroke (CHADS2VASC 2+), an anti-clotting medication such as warfarin or a novel oral anticoagulant (e.g., apixaban) is typically recommended.[1]
- Reasoning
Multiple guidelines clearly indicate that risk stratification based on the CHADS2/CHADS2VASC scoring systems is important when deciding how to approach a patient with atrial fibrillation. Furthermore, these guidelines differentiate risk (and therefore treatment) between 0 and 1 (0 is low risk, 1 is intermediate risk, and 2+ is high risk for stroke/systemic embolism). Of note, I am amenable to addition of this caveat (since CHADS2VASC (instead of CHADS2) technically gives a score of 1 for female sex but is unique in that anticoagulation is not recommended in this subgroup in the absence of other stroke risk factors (previously acknowledged multiple times above), it would be reasonable to specify CHADS2VASC 1 for men, 2 for women): "However, antithrombotic therapy is not recommended for female patients with no other risk factors of stroke." Or we can say CHADS2VASC score of 1 in men or 2+ in women to be more accurate to overcome the female sex point in the CHADS2VASC system. A CHADS2VASC score of 0 is low-risk (not achievable by women since a point is given for female sex). A CHADS2VASC score of 1 is low risk for women (since this point is only for female sex) but not for men. Therefore, it's an oversimplification to say CHADS2VASC score 1 is low-risk. It's only partially true and it's misleading to group them together this way in the lead. The zero and 1 scores should not be conflated either. I think better definitions of these groups are important in the lead.
1) Direct quote from the Japanese Cardiovascular Society: "- Anticoagulation therapy with dabigatran (Level of Evidence: B) or apixaban (Level of Evidence: A) should be performed in intermediate-risk patients with a CHADS2 score of 1." and "Patients with a CHA2 DS2 -VASc of 0 (low risk patients) should basically not receive anticoagulation as the incidence of embolic events is too low to justify the risk of intracranial hemorrhage associated with warfarin therapy. " This clearly shows that a CHADS2/CHADS2VASC score of 1 is considered intermediate risk (not low-risk which is CHADS2/CHADS2VASC score of 0).
1b) Doc's point above re: ACC/AHA guidelines differentiating 0 and 1 also reinforces the point that both would not be (and should not be) classified under the catchall term "low-risk" (obviously the risk differs since the approach does per their guidelines too).
2) ACCP guidelines also distinguish between 0/1: "For patients with AF, including those with paroxysmal AF, who are at low risk of stroke (eg, CHADS2 [congestive heart failure, hypertension, age ≥ 75 years, diabetes mellitus, prior stroke or transient ischemic attack] score = 0), we suggest no therapy rather than antithrombotic therapy" and "2.1.9. For patients with AF, including those with paroxysmal AF, who are at intermediate risk of stroke (eg, CHADS2 score = 1), we recommend oral anticoagulation rather than no therapy" and "2.1.10. For patients with AF, including those with paroxysmal AF, who are at high risk of stroke (eg, CHADS2 score = 2), we recommend oral anticoagulation rather than no therapy".
3) The CCS guideline clearly differentiates the risk of CHADS20/1: "The current CCS AF guidelines recommendations for patients with AF who are at low risk of SSE (age < 65 years, CHADS2 score of 0) are no antithrombotic therapy if there is no manifest vascular disease (CAD, peripheral vascular disease, or aortic plaque) and ASA 81 mg/d if vascular disease is present (Fig. 1).3 " and "In patients with AF who are aged ≥ 65 years or with CHADS2 score ≥ 1, OAC is indicated for stroke prevention.3"
4) As a counter to James' point about UptoDate, we generally do not rely on it in Wikipedia for our information. We should be consistent about this.
5) A brief discussion of the CHADS2 or CHADS2VASC score would not need to be complicated in the lead and would better delineate low/intermediate/high risk in the lead since this clearly changes management approach. TylerDurden8823 (talk) 10:08, 25 December 2017 (UTC)
References
Support
- Version 1
- Support Simpler and more accurate. Which score equals "low risk" varies in different sources. Nearly all source call women with a score of 1 low risk. Thus easier to describe treatment by risk rather than by score in the lead. Scores should go in the body of the text. Doc James (talk · contribs · email) 11:56, 25 December 2017 (UTC)
- Support The CHADxxxx wording is too specialized for an article lede (though may be good in the body). Alexbrn (talk) 12:00, 25 December 2017 (UTC)
- support agree w/ Alexbrn--Ozzie10aaaa (talk) 12:57, 25 December 2017 (UTC)
- Support as above. In the discussion I suggest slight rewording for clarity.JonRichfield (talk) 06:47, 26 December 2017 (UTC)
- Neutral as per my comments below with new proposed language. Version 1 isn't really "more accurate" but I'll agree that it's simplified. More discussion about CHADS2VASC is probably warranted in the article's body but I do think the lead could use a bit of rewording (per James' proposed version below) for additional clarity. We can probably close out the RFC now. TylerDurden8823 (talk) 07:56, 26 December 2017 (UTC)
- Support. The lead should use simple accessible language if possible. The risk classification system can be explained in the body of the article. Maproom (talk) 09:54, 26 December 2017 (UTC)
- Version 2
Discussion
From WP:DUE:
Neutrality requires that each article or other page in the mainspace fairly represent all significant viewpoints that have been published by reliable sources, in proportion to the prominence of each viewpoint in the published, reliable sources.
From WP:ASSERT:
When a statement is an opinion (e.g. a matter which is subject to serious dispute or commonly considered to be subjective), it should be attributed in the text to the person or group who holds the opinion.
That suggests strongly that the difference in guidance about the use of aspirin needs to be described and attributed in the body of the text. I don't believe it is our place to decide which guideline is "right" in order to exclude the other. That much detail belongs out of the lead, of course, but whatever wording is used, it should admit the fact that opinion remains divided at present about recommending aspirin. FWIW, version 1 has the simplest language, so I would find it preferable. --RexxS (talk) 14:30, 25 December 2017 (UTC)
- @TylerDurden8823 and Doc James: Please consider adding a short summary after the "Which of these sentences should go as a summary in the lead of this article?" sentence, but before the "Version 1" subheading, in accordance with WP:RFC#Statement should be neutral and brief; conclude it with either a full signature or a timestamp. This is to trim down the entry at Wikipedia:Requests for comment/Maths, science, and technology which is by no means brief. --Redrose64 🌹 (talk) 19:40, 25 December 2017 (UTC)
- User:TylerDurden8823 I have been thinking more about the concerns you mentioned. Agree that for low risk people the usual recommended treatment is nothing. Would this "For those at low risk of stroke, no specific treatment is typically required, though aspirin or an anti-clotting medications may occasionally be considered." better reflect this in your opinion? And than we keep "For those at more than low risk an anti-clotting medication is typically recommended." because those at intermediate risk should generally be anti-coagulated. Doc James (talk · contribs · email) 23:55, 25 December 2017 (UTC)
- Without strong feelings on the alternatives, I propose something like:
For patients at low risk of stroke it is usual to refrain from any specific treatment, though aspirin or anti-clotting medications may be advisable in doubtful cases.[1] For patients clearly at risk, anti-clotting medication is commonly appropriate, for example warfarins or direct oral anticoagulants.[1] JonRichfield (talk) 07:23, 26 December 2017 (UTC)
- Doc James, yes, the most recent version you suggested here sounds better. Jon, I think that version is a little too vague (what constitutes a "doubtful case"). TylerDurden8823 (talk) 07:53, 26 December 2017 (UTC)
- RexxS, the difference in the guidelines' recommendations regarding aspirin's utility (or lack thereof) is discussed in the body. I'm not suggesting we decide which guideline is "right", but I think it's clear that the AHA/ACC's guideline is the outlier/minority viewpoint when compared to the rest (this is further reflected in multiple literature reviews discussing these guidelines which explicitly state that aspirin is increasingly being stricken from such guidelines and our content should reflect what the literature really says). TylerDurden8823 (talk) 07:59, 26 December 2017 (UTC)
- Okay perfect. If that works for you User:TylerDurden8823 happy to see this closed aswell. Doc James (talk · contribs · email)
- Great, let's make the changes and close out the RFC. TylerDurden8823 (talk) 17:40, 26 December 2017 (UTC)
- Okay perfect. If that works for you User:TylerDurden8823 happy to see this closed aswell. Doc James (talk · contribs · email)
References
Erectile dysfunction
This needs adding. I tried to but I was told my reference source was inadequate. There is no similar source for female sexual dysfunction as far as I can see but there may be. The source I quoted referred not only to erectile issues but also to emotional and desire issues in males. 86.187.163.73 (talk) 23:35, 22 September 2018 (UTC)
This is the reference I used: https://onlinelibrary.wiley.com/doi/abs/10.1111/pace.12753 86.187.163.73 (talk) 23:38, 22 September 2018 (UTC)
- The paper you provide a link to is interesting - I was unaware of a strong association between erectile dysfunction and AF. Despite this, the Wikipedia guidelines e.g. WP:MEDRS discourage the use of primary sources such as the small observational study you cited and instead recommend using secondary sources such as review articles, meta-analyses, guideline documents, book chapters etc. As I understand it, well-written secondary sources are more likely to reflect a consensus of opinion from multiple potentially conflicting primary sources.
- If you can find secondary sources to back up your assertion that the majority of male patients with AF suffer erectile dysfunction then feel free to reinsert your (now appropriately cited) edit, probably as a subsection of Signs and Symptoms. Hope that helps. PeaBrainC (talk) 16:05, 24 September 2018 (UTC)
- Thank you for your guidance. I hope the links are now adequate. One of them was labelled spam by another Wikipedian. I have deleted it. 86.187.167.253 (talk) 17:09, 25 September 2018 (UTC)
- no those refs fail WP:MEDRS. A letter to the editor and a primary source are not OK per MEDRS. The spam link was unambiguous advertising and purely abusive of your editing privileges; trying to play that off as "was called spam" is dreadful. Jytdog (talk) 17:51, 25 September 2018 (UTC)
- PMID 30014525 is the kind of source we want. It finds an association, with lots of caveats. Jytdog (talk) 18:33, 25 September 2018 (UTC)
- OK. I would like to reinsert the erectile dysfunction with PMID 30014525. We assume good faith; thank you for correcting me. I am about to reinsert the piece. Best wishes. 86.187.169.65 (talk) 02:16, 26 September 2018 (UTC)
- Thank you for the pubmed link and again, thank you for your guidance. 86.187.169.65 (talk) 02:28, 26 September 2018 (UTC)
- You have lost the right to ask for good faith with your disgusting spamming. The content you added was not supported by the source.Jytdog (talk) 02:31, 26 September 2018 (UTC)
- OK, I will leave the matter. Best wishes to you. 86.187.169.65 (talk) 02:33, 26 September 2018 (UTC)
- You have lost the right to ask for good faith with your disgusting spamming. The content you added was not supported by the source.Jytdog (talk) 02:31, 26 September 2018 (UTC)
- Thank you for your guidance. I hope the links are now adequate. One of them was labelled spam by another Wikipedian. I have deleted it. 86.187.167.253 (talk) 17:09, 25 September 2018 (UTC)
Bad links
Some of the links are no longer valid. Nicmart (talk) 23:56, 28 September 2018 (UTC)
- Please be more specific. Jytdog (talk) 00:44, 29 September 2018 (UTC)
